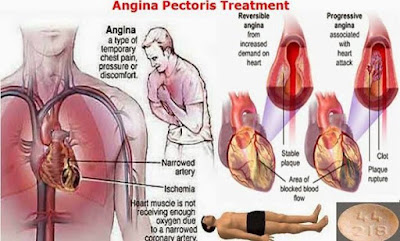
An anginal pain attack signals a transient hypoxia of the myocardium. As a rule, the oxygen deficit results from inadequate myocardial blood flow due to narrowing of larger coronary arteries.
The underlying causes are: most commonly, an atherosclerotic change of the vascular wall (coronary sclerosis with exertional angina); very infrequently, a spasmodic constriction of a morphologically healthy coronary artery (coronary spasm with angina at rest; variant angina); or more often, a coronary spasm occurring in an atherosclerotic vascular segment.
The goal of treatment is to prevent myocardial hypoxia either by raising blood flow (oxygen supply) or by lowering myocardial blood demand (oxygen demand) (A).
Factors determining oxygen supply.
The force driving myocardial blood flow is the pressure difference between the coronary ostia (aortic pressure) and the opening of the coronary sinus (right atrial pressure). Blood flow is opposed by coronary flow resistance, which includes three components.
(1) Due to their large caliber, the proximal coronary segments do not normally contribute significantly to flow resistance.However, in coronary sclerosis or spasm, pathological obstruction of flow occurs here. Whereas the more common coronary sclerosis cannot be overcome pharmacologically, the less common coronary spasm can be relieved by appropriate vasodilators (nitrates, nifedipine).
(2) The caliber of arteriolar resistance vessels controls blood flow through the coronary bed. Arteriolar caliber is determined by myocardial O2 tension and local concentrations of metabolic products, and is “automatically” adjusted to the required blood flow (B, healthy subject). This metabolic autoregulation explains why anginal attacks in coronary sclerosis occur only during exercise (B, patient). At rest, the pathologically elevated flow resistance is compensated by a corresponding decrease in arteriolar resistance, ensuring adequate myocardial perfusion. During exercise, further dilation of arterioles is impossible. As a result, there is ischemia associated with pain. Pharmacological agents that act to dilate arterioles would thus be inappropriate because at rest they may divert blood from underperfused into healthy vascular regions on account of redundant arteriolar dilation. The resulting “steal effect” could provoke an anginal attack.
(3) The intramyocardial pressure, i.e., systolic squeeze, compresses the capillary bed. Myocardial blood flow is halted during systole and occurs almost entirely during diastole. Diastolic wall tension (“preload”) depends on ventricular volume and filling pressure. The organic nitrates reduce preload by decreasing venousreturn to the heart.
Factors determining oxygen demand.
The heart muscle cell consumes the most energy to generate contractile force. O2 demand rises with an increase in
(1) Heart rate,
(2) Contraction velocity,
(3) Systolic wall tension (“afterload”).
The latter depends on ventricular volume and the systolic pressure needed to empty the ventricle. As peripheral resistance increases, aortic pressure rises, hence the resistance against which ventricular blood is ejected. O2 demand is lowered by β-blockers and Calcium-antagonists, as well as by nitrates.

No comments:
Post a Comment